Accurate medical coding is the backbone of a successful healthcare revenue cycle. Medical coding companies specialize in translating medical procedures, diagnoses, and treatments into universally recognized codes such as ICD-10, CPT, and HCPCS. These codes are essential for proper billing, insurance claims, and regulatory compliance.
Partnering with a professional medical coding company allows healthcare providers to improve billing accuracy, reduce claim denials, and focus on delivering high-quality patient care.
A medical coding company is a specialized service provider that handles coding for hospitals, clinics, and private practices. Their primary role is to ensure that every medical service or procedure is correctly coded according to industry standards. This ensures claims submitted to insurance companies are accurate, reducing the chances of delays or denials.
Medical coding companies employ certified coders who are experts in ICD-10, CPT, and HCPCS coding systems. These professionals stay updated with the latest changes in coding guidelines and healthcare regulations.
📞 Call/WhatsApp: +1 (561) 600-4443
📧 Email: info@backbonedatasolutions.com
🌐 Website: Visit Backbone Data Solution
A reliable medical coding company provides a range of essential services:
ICD-10 and CPT Coding
Accurate coding of diagnoses, procedures, and medical treatments for billing purposes.
Claim Auditing
Reviewing claims for errors before submission to prevent denials and ensure compliance.
Revenue Cycle Support
Helping healthcare providers maximize reimbursements by ensuring all services are coded correctly.
Compliance Management
Ensuring adherence to HIPAA and other healthcare regulations to avoid penalties.
Training and Consultation
Providing training to in-house staff and consultation on coding best practices.
Denial Management
Assisting providers in correcting coding errors on denied claims and resubmitting them for payment.
Outsourcing coding tasks to a medical coding company has several advantages:
Improved Accuracy: Certified coders reduce errors and ensure claims are submitted correctly.
Faster Reimbursements: Accurate coding leads to quicker claim approvals and payments.
Cost Savings: Reduces the need for in-house coding staff and related overheads.
Regulatory Compliance: Ensures adherence to HIPAA and other medical coding regulations.
Focus on Patient Care: Healthcare providers can focus on delivering quality care instead of administrative tasks.
Access to Expertise: Coding companies employ experienced professionals who stay updated on coding changes and payer requirements.


Even with a medical coding company, challenges in medical coding can arise:
Frequent Updates to Coding Guidelines: ICD-10 and CPT codes are regularly updated, requiring ongoing training.
Complex Medical Records: Incomplete or unclear patient records can make accurate coding difficult.
Claim Denials: Errors in coding can lead to rejected insurance claims, requiring additional follow-up.
Regulatory Compliance: Non-compliance with HIPAA or payer-specific rules can result in penalties.
Technological Integration: Coding companies must ensure compatibility with various healthcare management systems.
Technology has transformed medical coding companies in several ways:
Electronic Health Records (EHR): EHR systems streamline access to patient data, improving coding accuracy.
Coding Software: Automated software tools help coders quickly assign correct codes.
Artificial Intelligence (AI): AI can detect potential errors and inconsistencies in medical records.
Cloud-Based Systems: Allow remote coders to securely access patient data and work efficiently.
Analytics & Reporting: Coding companies use analytics to track claim performance and optimize revenue cycles.


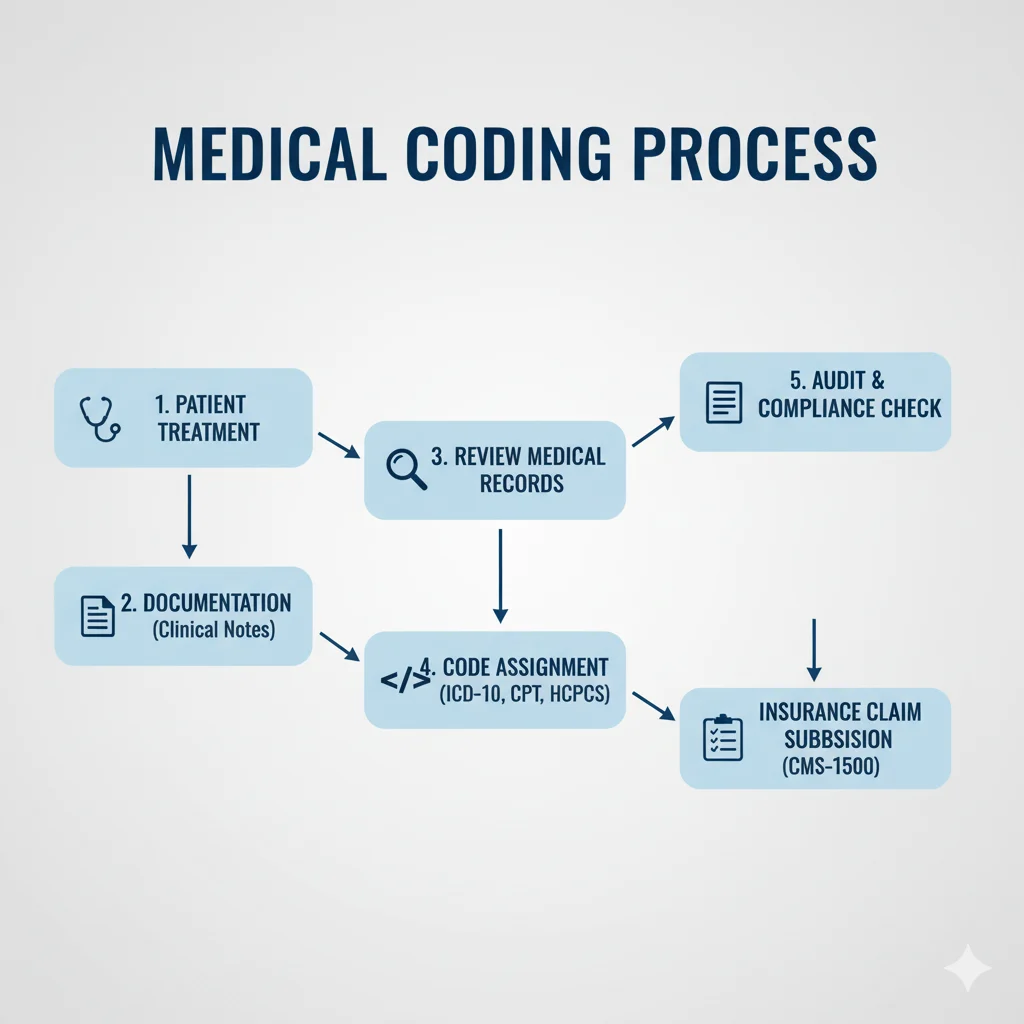
Collect Patient Records: Accurate documentation of diagnoses, treatments, and procedures.
Verify Documentation: Ensure all information is complete and consistent.
Assign Codes: Using ICD-10, CPT, and HCPCS coding systems for accurate claim preparation.
Submit for Billing: Forward coded information to billing teams or medical billing companies.
Handle Denials: Correct coding errors on denied claims and resubmit them.
Generate Reports: Provide insights into coding efficiency, claim performance, and revenue.
By outsourcing to a medical coding company, healthcare providers can ensure accurate coding, reduce errors, and improve their overall revenue cycle.
When selecting a medical coding company, consider these factors:
Certification & Expertise: Coders should be certified (e.g., CPC, CCA) and experienced in your specialty.
Compliance: Must adhere to HIPAA and industry coding standards.
Technology: Use of advanced coding software and EHR integration.
Customer Support: Quick response to queries and claim-related issues.
Cost & ROI: Transparent pricing and measurable improvement in coding accuracy and reimbursements.
Partnering with the right medical coding company ensures a seamless, accurate, and efficient coding process that benefits both providers and patients.

We value every inquiry and understand that your time is important. Whether you have a question about our services, need more details before making a decision, or simply want to share your feedback, our team is always ready to assist you. Our goal is to provide clear, prompt, and helpful responses so that you feel supported at every step.
Send us a message and we will respond as quickly as possible. Our team is always ready to assist you with queries, guidance, or support so that you receive the right information without any delay.
