Efficient medical billing isn’t just about faster payments—it’s about accuracy, compliance, and a healthy revenue cycle. A streamlined medical billing workflow helps healthcare practices reduce denials, improve cash flow, enhance patient satisfaction, and lower administrative burden.
Whether you're running a small clinic or a multi-specialty healthcare center, improving billing efficiency can immediately elevate your financial performance. In this guide, we’ll break down the best strategies to enhance your medical billing workflow, backed by expert insights and real-world practicality.
What Is a Medical Billing Workflow?
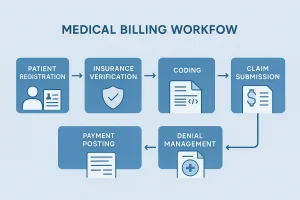
A medical billing workflow is the complete process used to collect payments, submit claims, verify insurance, code services, and manage reimbursements in a healthcare facility.
A medical billing workflow is a structured process that includes patient registration, insurance verification, coding, claim submission, payment posting, and denial management.
Why an Efficient Medical Billing Workflow Matters
A smooth workflow ensures:
- Faster claim approvals
- Fewer mistakes
- Reduced denials
- Higher revenue
- Better patient experience
- Less administrative overload
When the process is efficient, providers spend less time chasing payments and more time caring for patients.
1. Strengthen Patient Registration & Data Accuracy
The first step of every medical billing workflow is collecting patient details. Errors here lead to claim denials later.
Tips:
- Verify patient demographics
- Confirm insurance details
- Capture ID and insurance card images
- Update information every visit
2. Improve Insurance Eligibility Verification
One of the biggest workflow delays happens when insurance information is outdated or incorrect.
Ways to improve:
- Use automated eligibility tools
- Verify coverage before every appointment
- Check co-pay, deductible, and prior authorization needs
This step alone can significantly strengthen your medical billing workflow.

3. Ensure Accurate Medical Coding
Coding errors = denials, delays, and compliance risks.
Tips for better coding:
- Train coders regularly
- Update ICD-10, CPT, HCPCS codes
- Use certified coders
- Implement coding audits
Accurate coding protects revenue and enhances the medical billing workflow from the inside out.
4. Implement Clean Claim Submission Practices
A “clean claim” is a claim accepted on the first submission—no errors, no corrections needed.
Make claims cleaner by:
- Using claim-scrubbing tools
- Verifying modifiers
- Checking payer-specific rules
- Ensuring documentation accuracy
The more clean claims you submit, the stronger your medical billing workflow becomes.
5. Use Automation to Reduce Manual Tasks
Automation improves speed and accuracy. In modern RCM, automation handles tasks like:
- Eligibility verification
- Claim scrubbing
- Denial alerts
- Payment posting
- Coding suggestions
Automation minimizes human error, saving time and boosting workflow efficiency.

6. Strengthen Documentation & Provider Notes
Strong documentation = accurate coding = faster claims.
Improve documentation by:
- Training providers on required details
- Using templates
- Encouraging real-time documentation
- Conducting documentation audits
Poor notes create workflow bottlenecks—especially during coding and claims processing.
7. Enhance Communication Between Billing & Clinical Teams
Miscommunication leads to billing delays.
Fix this by:
- Weekly billing huddles
- Shared digital communication channels
- Clarifying documentation and authorization requirements
A united team leads to a seamless medical billing workflow.
8. Track Key Performance Indicators (KPIs)
Measuring performance reveals workflow gaps.
Track these KPIs:
- AR days
- Claim denial rate
- First-pass acceptance rate
- Net collection rate
- Average reimbursement time
Smart analytics make your medical billing workflow scalable and predictable.

9. Improve Denial Management Processes
Denials are inevitable—but weak denial management hurts revenue.
Improve denial handling:
- Identify root causes
- Resolve within 48–72 hours
- Maintain a denial log
- Appeal eligible claims
- Train staff based on trends
A strong denial management system strengthens the entire medical billing workflow.
10. Consider Outsourcing to a Medical Billing Company
If your practice is overwhelmed, outsourcing can dramatically improve workflow efficiency.
Benefits:
- Fewer errors
- Faster payments
- Compliance support
- Certified coders
- 24/7 billing coverage
- Reduced administrative burden
Outsourcing helps practices focus on patient care while experts manage the medical billing workflow.

Frequently Asked Questions
Q1: What slows down a medical billing workflow?
Incorrect patient data, poor documentation, coding errors, and insurance delays.
Q2: How can automation improve billing workflow?
Automation reduces manual tasks, improves accuracy, and speeds up claim submission.
Q3: What’s the fastest way to reduce claim denials?
Accurate eligibility checks, coding updates, and clean claim scrubbing.
Q4: Should small clinics outsource billing?
Yes — it reduces workload and improves efficiency if staff is overwhelmed.
A well-structured medical billing workflow is essential for a healthy revenue cycle. From accurate patient data to automated claim processing and strong denial management, every step plays a vital role in ensuring your practice gets paid faster and more consistently.
By implementing the tips in this guide—and considering professional outsourcing—you can create a workflow that’s efficient, compliant, and future-ready.
Author Info
Author: Mangesh
Last Updated: November 2025
Category: Home Appraisal & Property Valuation
Follow Us: facebook.com | instagram.com | linkedin.com | BackBoneDataSolutions.com