Claim denials are one of the biggest challenges healthcare providers face. They delay payments, disrupt cash flow, create administrative stress, and directly impact revenue. This is why many clinics turn to medical billing experts who know exactly how to reduce claim denials using structured processes and advanced tools.
In this guide, we break down how medical billing companies tackle denials, the steps they follow, and why partnering with experts can transform your revenue cycle.
Understanding Why Claim Denials Happen
Before understanding how professionals reduce claim denials, it’s important to know the common triggers:
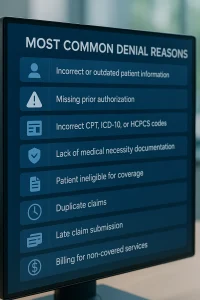
Most Common Denial Reasons
- Incorrect or outdated patient information
- Missing prior authorization
- Incorrect CPT, ICD-10, or HCPCS codes
- Lack of medical necessity documentation
- Patient ineligible for coverage
- Duplicate claims
- Late claim submission
- Billing for non-covered services
Medical billing companies analyze these patterns and use proven workflows to eliminate root-cause errors.
1. Accurate Patient Registration & Eligibility Checks
One of the most effective ways to reduce claim denials is by starting right at the front desk.
How Billing Companies Ensure Accuracy
- Real-time eligibility verification
- Confirm insurance coverage dates
- Check co-pays, deductibles, and plan limitations
- Validate policy numbers and spelling of names
- Identify need for referrals or authorizations
Snippet:
70% of healthcare claim denials are caused by errors during patient registration and eligibility verification.
2. Ensuring Proper Documentation Before Claim Submission
Medical billing companies emphasize documentation accuracy because even small gaps can cause major delays.
They ensure:
- Doctor notes match billed procedures
- Medical necessity is clearly documented
- All supporting files (labs, imaging, referrals) are attached
- Procedures align with payer requirements
This prevents avoidable denials due to insufficient content.
3. Cleaner Coding Through Certified Coders
Coding mistakes are one of the top reasons claims get rejected. To reduce claim denials, companies hire certified coders (CPC, CCS, RHIT) who understand:
- CPT codes
- ICD-10 diagnosis codes
- HCPCS service codes
- Modifiers
- NCCI edits
- Payer-specific rules
They run every claim through strict coding audits to catch errors before submission.

4. Automated Claim Scrubbing Tools
Modern billing companies rely on AI-powered scrubbers to catch issues instantly.
Claim scrubbers detect:
- Diagnosis-procedure mismatches
- Missing modifiers
- Wrong place of service codes
- Invalid provider NPI
- Payer-specific coding conflicts
This automated layer drastically helps reduce claim denials even before claims reach the payer.
5. Pre-Submission Quality Control (QC) Checks
Companies follow a structured QC process to ensure error-free claims.
QC Steps Include:
- Coding verification
- Documentation completeness review
- Matching notes with billed procedures
- Validating insurance rules
- Ensuring timelines are met
This step alone can increase first-pass acceptance rates significantly.
6. Submitting Claims on Time to Avoid Timely Filing Denials
Every insurance company has a strict claim submission window, often 30–90 days. Miss it—and the claim is denied permanently.
Billing companies use:
- Automated reminders
- Claim tracking systems
- Daily submission workflows
- Dedicated staff for follow-ups
These systems ensure no claim is ever late.

7. Monitoring Claims with Real-Time Tracking Tools
Once submitted, claims are continuously tracked to detect red flags early.
Tracking Tools Identify:
- Pending status
- Requests for additional information
- Suspended claims
- Rejected claims
The earlier issues are detected, the easier it is to reduce claim denials.
8. Immediate Handling of Rejected Claims
A rejected claim is one that insurance does not accept due to formatting or technical issues—not because the service was denied.
Billing companies:
- Correct errors immediately
- Resubmit the same day
- Avoid delays that may lead to denials
Quick action improves overall reimbursement success.
9. Aggressive Denial Management & Appeals
Denied claims require professional handling.
Billing companies appeal denials by:
- Reviewing denial codes
- Gathering missing documents
- Writing appeal letters
- Providing supporting medical necessity evidence
- Escalating with payer representatives
Their systematic approach helps reduce claim denials over time by fixing recurring problems.

10. Trend Analysis & Root-Cause Reporting
Data analysis plays a major role in preventing future denials.
Companies generate:
- Monthly denial trend reports
- Recurring error patterns
- Provider documentation insights
- Coding improvement recommendations
This creates long-term improvement rather than temporary fixes.
11. Training Providers & Staff to Avoid Future Denials
Billing companies also train clinical and front-desk teams on:
- Documentation accuracy
- Proper coding habits
- Insurance rules
- Pre-authorization requirements
- Industry updates
Education is one of the strongest long-term tools to consistently reduce claim denials.
Benefits of Working with a Medical Billing Company to Reduce Claim Denials
Working with experts helps you:
- Increase first-pass claim approval rate
- Speed up reimbursements
- Reduce administrative workload
- Prevent revenue leakage
- Improve documentation quality
- Strengthen your overall revenue cycle

Frequently Asked Questions
1. What is the fastest way to reduce claim denials?
Accurate eligibility checks and clean claim submission reduce most denials.
2. Why do insurance companies deny claims?
Common causes: coding mistakes, missing documents, ineligible patients, incorrect info.
3. Can denied claims be appealed?
Yes. Billing companies specialize in writing appeal letters and submitting documentation.
4. How do billing companies improve claim accuracy?
Using certified coders, automated scrubbers, audits, and QC checks.
5. Does outsourcing billing reduce claim denials?
Yes—outsourced experts focus entirely on accuracy, compliance, and payer rules.
Reducing claim denials is not about luck — it’s about consistency, accuracy, and expertise. Medical billing companies use structured systems, trained professionals, and advanced tools to ensure claims are submitted correctly the first time. By partnering with experts, healthcare providers improve revenue, reduce stress, and strengthen their entire practice workflow.
Author Info
Author: Mangesh
Last Updated: November 2025
Category: Home Appraisal & Property Valuation
Follow Us: facebook.com | instagram.com | linkedin.com | BackBoneDataSolutions.com